On Monday morning of July fifteenth, my alarm began going off at four fifteen. I got up and stumbled into the shower to wash my body with Hibiclens skin cleanser in preparation for my surgery which was to take place at seven thirty. While washing, my mind was all over the place. Would this surgery be like last time? Would I have any trouble with the anesthesia? Would I be nauseous? Was it going to hurt worse? Why did I decide to do this in the first place? I pushed all the questions aside, because I knew exactly why I had decided on this particular surgery. This surgery meant no foreign bodies in my body. This surgery meant less risk of infection. This surgery meant less risk of rejection. This surgery would lead to the most natural results. Most importantly, this surgery was the one that I believed would leave me feeling the most like me. I got out of the shower, pulled my hair back, and got dressed. We needed to leave soon if we were going to get there on time.
On the way to City of Hope I know that Patrick (my husband) and I had conversations. However, what those conversations were about has escaped me. The surgery was just looming over me like a dark gray thundercloud with a teeny tiny rainbow. I just wanted to get to City of Hope and get it over with before I lost my nerve. I’m not sure if I was more nervous with this surgery over the bilateral mastectomies. I think it was just a different kind of nervous. With the bilateral mastectomies, it was a necessary surgery for my literal survival. They had to get the cancer out, so I just really didn’t have a choice. For the reconstruction, a surgery was going to be necessary, it just wasn’t absolutely required to be this one. So because of that, leading up to the surgery for the reconstruction I always felt like I had an out if I wanted to take it. But I drew myself up by my bootstraps, and we walked into City of Hope that morning right on time (after a failed attempt to come in the wrong door 
Much like the first surgery, once we got checked in I switched over to my glasses from my contacts and waited nervously for them to call me back. They didn’t really take long at all. Unlike the last surgery, they let both Patrick and Karyn (my sister) come back with me while they got me prepped and ready. For the bilateral mastectomies, they only allowed one person at a time to be with me. Luckily I had already had a PICC line put in the Friday before the surgery, so I didn’t have to deal with them adding any iv’s (although they apparently did add an IV during the surgery for some reason in the same arm). The weirdest prep they did was to put me in a gown that was attached to what looked like a vacuum hose. Instead of sucking air out, this hose pumped warm almost hot air into the gown. I didn’t complain because I was a little chilly, but I definitely asked what it was about. It turns out that there is research to support better outcomes for this surgery for patients who wore this gown leading up to the procedure. It was pretty interesting stuff. It wasn’t long after they got the gown on me that the nurse was pushing the “don’t care” medicine in my PICC line. I know that they were taking me to get a abdominal nerve block in my back, but I absolutely don’t remember them doing it.

The next thing I knew, I was awake, hot, and in a mild amount of pain around my abdomen. I was also in a strange position. I had to lay with the head of the bed elevated as well as the feet, and I had triangle wedges with pillows on them under my knees. The pain wasn’t too much to handle, but it was definitely more than the previous surgery. I was hot because the room had to be kept at eighty degrees at all times to promote good blood flow and healing. When I woke up, they let me know that I would be stuck in the bed for the rest of Monday, all of Tuesday, and Tuesday night. They would remove my Foley catheter on Wednesday and start getting me out of the bed. So, the rest of Monday and Tuesday are pretty much a blur. I remember having an awful headache that we just couldn’t get rid of and lasted for about 4 days. I remember them impressing upon me how important it was for me to start eating and getting in good calories. Most of all I remember that they had to check the implanted flaps with a doppler every single hour including through the night, so I didn’t really get much sleep.
Wednesday was better as far as progress was concerned, because I was able to get out of the bed and move over to the recliner or the bedside commode. I was more clearheaded although I still had the headache, and my appetite was slowly beginning to come back.
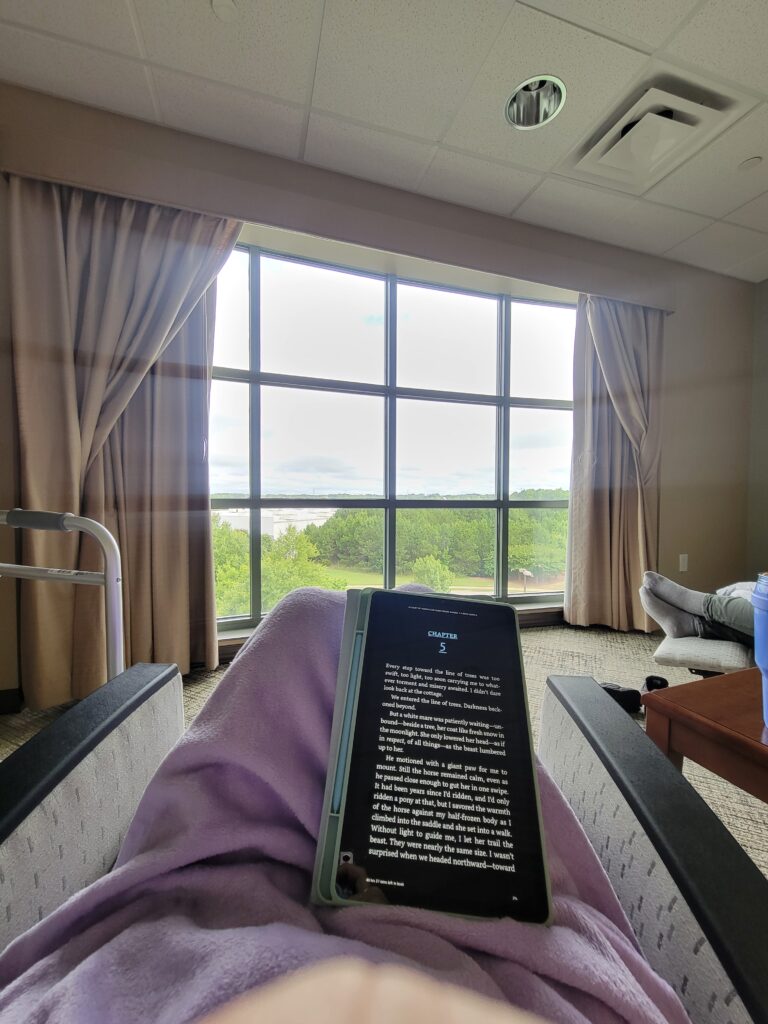
Thursday was a big day for progress! On Thursday, they brought me a walker and begin teaching me how to walk with it. Let me explain the need for the walker after this surgery. To do that, I will give a quick synopsis of the surgery I had again. Basically, the plastic surgeon (Dr. Durden) cut out the skin and fat tissue of my abdomen from belly button down to pubic bone and hip to hip. He examined the left and right side of the abdominal skin and fat tissues to see what parts would best be used to reconstruct my breasts. He needed tissue that had good blood vessels that he could attach to the vessels in my chest so that the tissue would remain living. Once he determined the parts best used, he cut them out and transplanted them underneath my original breast skin to reconstruct the breast. After he cut out the part of my abdomen to be used for the surgery, he pulled the remaining skin and tissue of my stomach area down to meet the skin and tissue at my pubic bone, and stitched them together. He also had to make a small incision to bring my belly button back through and stitch it into place. So to give the big picture on incisions that are currently healing, I have two incision lines on each breast because my original breast skin was stitched to the skin of the abdominal flap transplant which was then stitched to the skin of my chest. There is an incision all the way around my belly button, and there is the longest incision across my lower abdomen from hip to hip. My torso almost looks like a smiley face! 


Friday was discharge day! My headache had finally abated and I was ready to get out of the eighty degree room! Around two or three in the afternoon, they were ready to wheel me to my room. Just a short hop, jump, and a skip away and we were there in the blessed seventy five degree hotel room. I have now been in the hotel for a week and a day and I am super familiar with the City of Hope building. I have covered almost every inch of the building I have access to during my stay, including the roof! I have been very fortunate to have wonderful family members that have helped me out while I have been here. My sister Karyn was with me for the ICU stay and the first weekend, my niece Brittany stayed with me for two days, and my sister Megan has been with me since and will be with me until I leave this coming Friday. Patrick and the boys have been to visit me multiple times which helps me to miss them just a little bit less. I’ve gotten pretty good at zooming around here with the walker. I was told once that I was going to get a ticket and another time I was told, “No running in the hallways!” 😂 City of Hope has not only positive friendly staff, but they also have positive friendly patients as well.
The big question: Would I do it again knowing what I know now? Absolutely. I am no longer in any pain. I believe the last time I took Tylenol or Ibuprofen was around last Tuesday. The walker isn’t really too big of a deal. We have had small excursions over to Ashley Park and to get pedicures, and I have gotten around just fine. One of the most annoying things about these types of surgeries is the surgical drains. For the bilateral mastectomies, I had two that I had to deal with for five weeks. To maintain the drains, I have to use an alcohol wipe to pinch the cord leading to the drain and then pull it down the cord to make any liquid go into the drain at the end. I then have to empty the drain’s contents into a cup to get the measurement of the liquid and notate it. This has to be done twice a day. Well, with this surgery I was blessed with SIX drains… Luckily at my follow up appointment on Friday the twenty-seventh, they were able to pull four of the drains, so now I only have two to deal with. All of that to say, I’m doing great! I’m healing well and excited to get home to my family soon. Thank you to everyone for your thoughts, vibes, and prayers. Without the help from our village, this all would have not been possible! It’s crazy to think that from diagnosis to last major surgery and complete treatment (outside of adjuvant therapy) has been less than a year. That is so wild to me, but I couldn’t be happier to be past it and healing. Enjoy some photos of how things have been here at City of Hope!